-
Loss of awareness
-
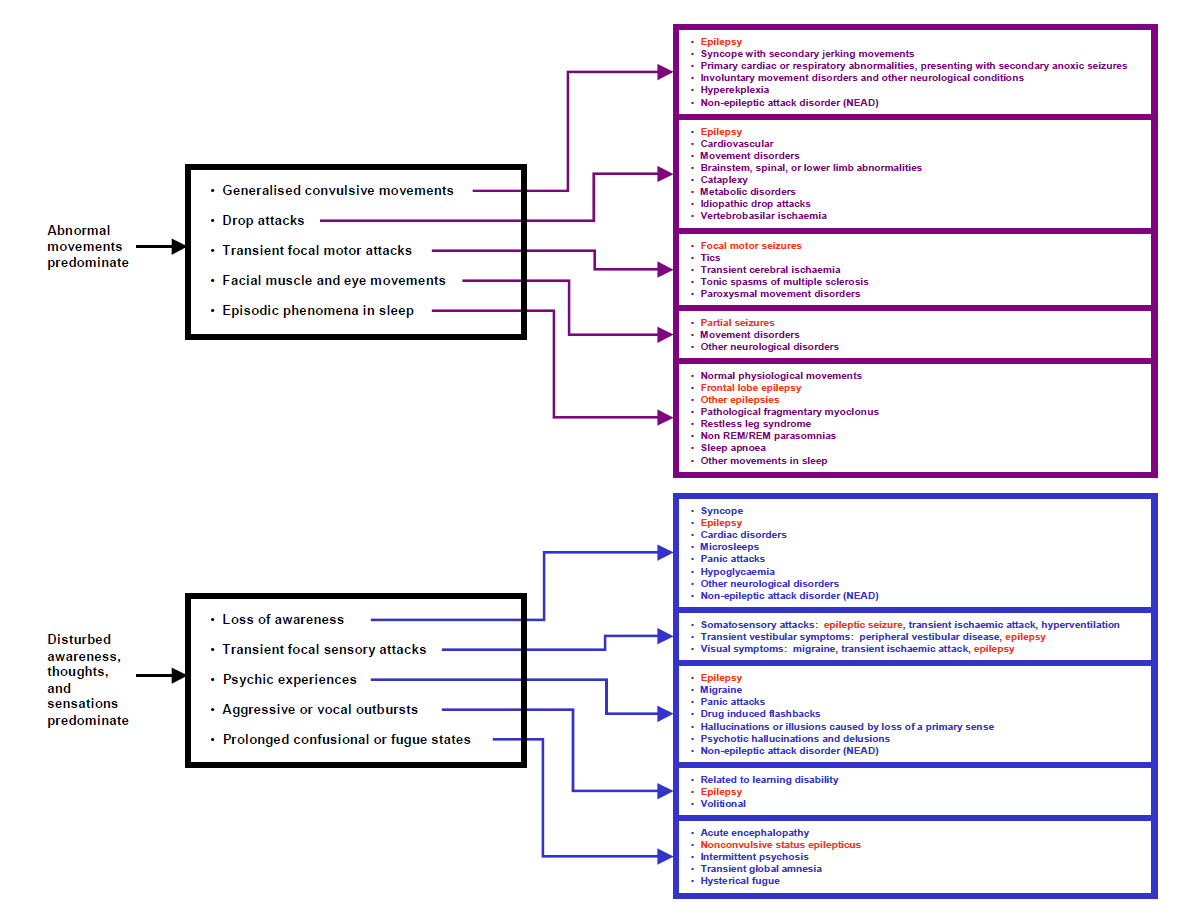
Generalised convulsive movements
-
Drop attacks
-
Transient focal motor attacks
-
Transient focal sensory attacks
-
Facial muscle and eye movements
-
Psychic experiences
-
Aggressive or vocal outbursts
-
Episodic phenomena in sleep
-
Prolonged confusional or fugue states
Epilepsy
3 most common causes Syncope, Epilepsy, Cardiac arrythymia
- Presyncope: Weakness, Dizziness, light headedness or "graying out" of consciousness without loss of postural tone
- Syncope: a flaccid motionless episode of loss of consciousness (LOC) for seconds to minutes. types and symptoms of syncope
- In reality none of the seizures actually cause this
- Generalized tonic–clonic seizures have obvious motor manifestations
- myoclonic seizures are very short jerks with no detectable LOC
- atonic seizures may cause abrupt falls but no prolonged LOC
- complex partial seizures or absence seizures cause alterationof awareness butnot limp motionless LOC.
- Episodes of LOC with eyes closed for several seconds to minutes are either psychogenic or syncopal
- However, confusion arises as syncopal events can appear "convulsive"
- they in fact frequently involve brief body jerks.
- Motor symptoms associated with syncope are clonic- or myoclonic-like, tend to last only a few seconds, and terminate once the patient is horizontal, in sharp contrast to the typical generalized tonic–clonic seizure duration of 30 to 90 seconds
- Most common mechanism for syncope (vasovagal response)
- typically triggered by clear precipitants (e.g., pain such as inflicted by medical procedures, emotions, cough, micturition, hot environment, prolonged standing, exercise)
- Other historical features that favor syncope
- presyncopal prodromes (malaise, sweating, dizziness, lightheadedness, nausea, chest pain, palpitations), as well as age and a history of cardiovascular disease.
- Historical features that favor seizures
- tongue biting, head turning, posturing, urinary incontinence, cyanosis, prodromal déjà-vu, and postictal confusion
- Point based score system [94% sensitivity and 94% specificity] link
- EEGs are sensitive to decreased cerebral blood flow -> by the time LOC occurs -> EEG changes are present -> delta slowing and suppression
- seizure may present with loss of awareness as the sole reported feature
- Typical absences involve arrest of activity, reduced or lost awareness, eyelid blinking or twitching, and sometimes small myoclonic facial or limb jerks, or brief facial automatisms such as lip smacking or chewing. Often occur many times per day. There may also be isolated myoclonic jerks.
- Atonic seizures usually give rise to drop attacks but may appear to cause blank spells if the patient is sat or laying down and so cannot fall.
- Complex partial seizures may cause loss of awareness with few if any other features.
Chronic daytime sleepiness with episodic sleep attacks; also cataplexy, sleep paralysis, hypnagogic and hypnopompic hallucinations. more
Intense fear with palpitations, diaphoresis, choking sensation, shortness of breath, chest pain, nausea, dizziness, derealization, fear of dying/losing control, parasthesias, chills. Occasionally these preludes may be forgotten, and attacks present with loss of awareness. more
Rare except in patients for treated diabetes mellitus; very rare insulin secreting tumor; history of a missed meal prior to the attack. more
Head injury -> LOC and / or amnesia. Occasionally, structural CNS abnormalities may present with episodes of loss of awareness.more
Isolated episodes of loss of awareness may also be caused by abuse of psychotropic drugs or other substances.
This page was last updated on 16/12/18.